Table of contents:
- Which symptoms require a dermatologist’s consultation?
- Symptom 1: A mole or spot that is changing
- Symptom 2: Persistent itching with no obvious cause
- Symptom 3: A rash that doesn’t go away or spreads
- Symptom 4: Skin cracks that take a long time to heal
- Symptom 5: Peeling or excessive skin dryness
- Symptom 6: Painful, fluid-filled, or pus-filled breakouts
- Symptom 7: Hair loss or the appearance of bald patches
- Symptom 8: Changes in skin tone or hyperpigmentation
- Symptom 9: Changes in nails and the skin around them
- Symptom 10: Lumps or “bumps” under the skin
- Why you shouldn’t delay a visit to a dermatologist
When unusual spots, rashes, or persistent itching appear on the skin, many people try to handle it on their own: they change their skincare routine, buy a “universal” ointment, or follow advice found online. However, the skin rarely “gets it wrong” without a reason. It is often the first to react to infections, allergic reactions, immune system dysregulation, hormonal fluctuations, and metabolic problems. What initially looks like a minor cosmetic issue can sometimes be a symptom of a condition that requires professional diagnosis and treatment.
It is important to understand that different skin disorders may look very similar. For example, redness or scaling that appears the same at first glance may be related to contact dermatitis, a fungal infection, or psoriasis—and the treatment approach will be different in each case. Self-treatment in these situations can “blur” the clinical picture, lead to complications, or prolong the course of the disease.
In this article, we have collected 10 symptoms you should not ignore. We will explain which signs may be concerning, why they occur, and when seeing a doctor should be as prompt as possible.
Which symptoms require a dermatologist’s consultation?
Not all skin changes are dangerous, but there are signs that require a doctor’s attention. These are symptoms that do not resolve on their own, worsen over time, or appear without an obvious trigger.
Warning signs include:
- rashes, spots, or growths that persist for several weeks;
- changes in color, shape, or size of skin lesions;
- a rash spreading to new areas of the body;
- the onset of pain, itching, burning, or a feeling of tightness;
- no improvement with self-care or self-treatment.
Particular attention is needed when skin changes are not linked to new cosmetics, household chemicals, or dietary factors. In such cases, symptoms may be a manifestation of a dermatologic or systemic condition.
Below, we review 10 key symptoms for which seeing a dermatologist is necessary, even if your overall well-being remains satisfactory.
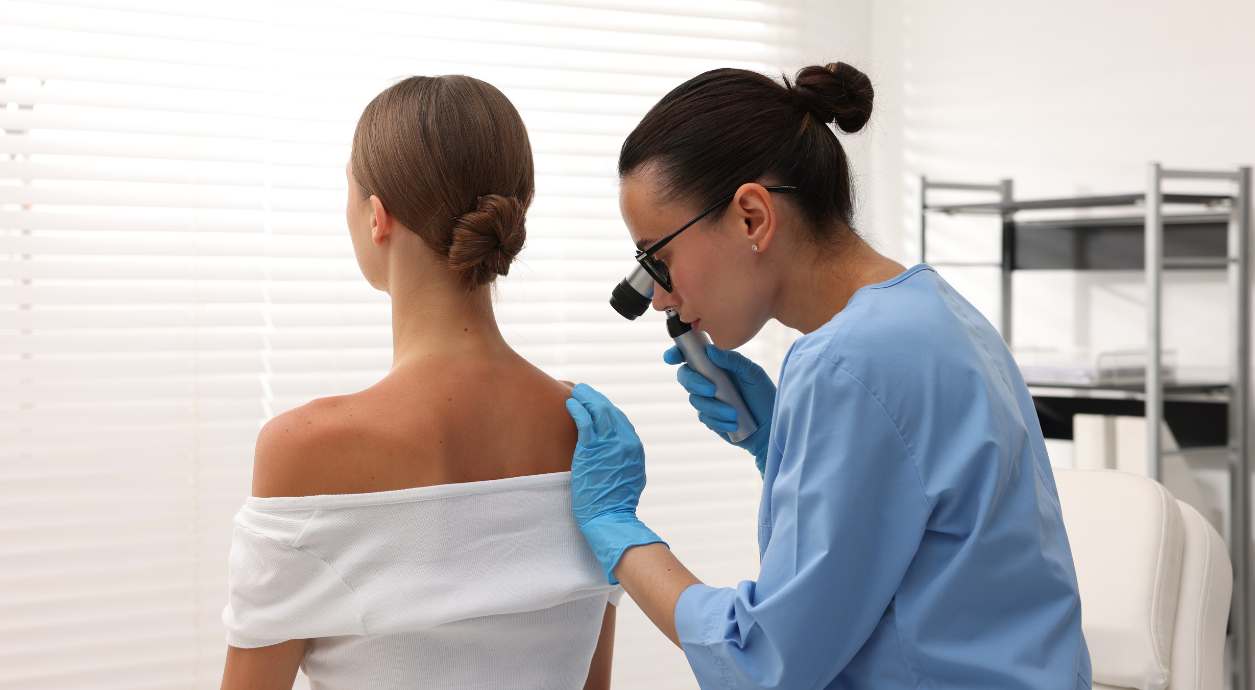
Symptom 1: A mole or spot that is changing

Pigmented lesions are present in most people and, in many cases, do not pose a threat. However, any change in a mole or spot requires careful attention because it may be an early sign of a malignant process.
Changes that are especially concerning include:
- new asymmetry or a change in the usual shape;
- uneven, “blurred,” or notched borders;
- color changes or multiple shades within one lesion;
- an increase in size or thickening;
- bleeding, itching, or inflammation around the spot.
Even if a mole has existed for many years and has not previously caused concern, its transformation is a reason to consult a dermatologist. During the examination, the doctor can perform dermatoscopy, which allows you to assess the structure of the mole in detail, identify dangerous changes at an early stage and determine further tactics of observation or treatment. Timely examination and diagnosis allow you to exclude dangerous conditions or detect them at an early stage, when treatment is most effective.
Symptom 2: Persistent itching with no obvious cause
Itchy skin is not always accompanied by a rash or redness, but persistent itching is an important signal that should not be ignored. If itching lasts for several weeks, intensifies, or interferes with daily life, a dermatologist’s consultation is needed.
Possible causes of persistent itching include:
- contact or atopic dermatitis;
- early-stage psoriasis;
- allergic skin conditions without a pronounced rash;
- dry skin with a disrupted protective barrier;
- systemic disorders, including endocrine or metabolic problems.
It is especially concerning if itching does not improve after using moisturizers or anti-itch creams. Self-treatment in such cases often only temporarily masks the symptom and does not address the cause.
A dermatologist’s examination helps determine whether itching is related to a local skin disorder or is a sign of deeper changes in the body that require a comprehensive approach to treatment.
Symptom 3: A rash that doesn’t go away or spreads
Skin rashes can appear for many reasons and do not always require urgent intervention. However, if a rash does not resolve within a few days, changes in character, or spreads to new areas of the body, this is a reason to see a dermatologist.
Concerning signs include:
- a rash that persists for more than 7–10 days;
- new lesions appearing or merging into larger areas;
- no effect from anti-allergy medications;
- worsening overall condition together with the rash.
It is important to understand that different types of rashes may look similar but have completely different causes—allergic, infectious, fungal, or autoimmune. That is why self-diagnosis is often inaccurate and may lead to inappropriate treatment.
Symptom 4: Skin cracks that take a long time to heal
Skin cracks are often seen as a result of dryness or mechanical irritation. However, if they occur regularly, heal poorly, or are accompanied by pain and inflammation, this may indicate a dermatologic issue or a systemic disorder.
Conditions to rule out include:
- chronic dermatoses, including eczema;
- metabolic disorders, including diabetes mellitus;
- infectious skin lesions;
- prolonged irritation or contact with aggressive substances.
Cracks most commonly appear on the hands, heels, around the fingers, or in skin folds. When the protective barrier is damaged, the risk of bacterial or fungal infection increases, which can complicate skin conditions.
If cracks do not heal over a prolonged period or keep recurring, a dermatologist’s consultation is necessary to identify the cause and select effective treatment.
Symptom 5: Peeling or excessive skin dryness
.jpg)
Dryness and peeling are not always related only to cold weather or dry indoor air. If these signs become persistent, worsen, or cause discomfort, it is worth seeing a dermatologist.
Possible causes include:
- disruption of the skin barrier;
- seborrheic dermatitis;
- rosacea;
- psoriasis in early or subtle forms;
- atopic and other chronic skin diseases;
- internal disorders, including hormonal or metabolic problems.
A particularly concerning situation is when dryness does not improve after changing skincare or using moisturizers, and when peeling appears locally—on the face, scalp, elbows, or knees.
In such cases, it is important not to mask symptoms with cosmetics but to determine the cause.
Symptom 6: Painful, fluid-filled, or pus-filled breakouts
Breakouts that are painful, filled with fluid, or contain pus require special attention. Such manifestations rarely resolve on their own and often indicate an infectious or inflammatory process.
Most common causes include:
- viral infections, including herpes;
- bacterial skin diseases, including impetigo;
- inflammatory forms of acne;
- secondary infection in chronic dermatoses;
- reduced local or general immunity.
Blisters that rapidly enlarge, are painful, rupture, or are accompanied by fever are particularly dangerous. Self-treatment in such cases may lead to the spread of infection and complications.
A dermatologist’s evaluation is needed to determine the nature of the rash, assess the depth of involvement, and start treatment in time to prevent progression.
Symptom 7: Hair loss or the appearance of bald patches
.jpg)
Increased hair shedding or areas of noticeable thinning may be a symptom of skin disorders or broader disturbances in the body.
Possible causes include:
- diffuse hair shedding due to stress or hormonal changes;
- autoimmune alopecia areata;
- fungal infections of the scalp;
- chronic inflammatory skin conditions;
- impaired nourishment of hair follicles.
Particular attention is needed if you notice clearly defined bald patches, brittle hair, itching, or scaling of the scalp. In such cases, cosmetic products do not solve the problem and may only conceal its manifestations.
A dermatologist’s consultation is needed to identify the cause of hair loss, distinguish temporary conditions from chronic processes, and select an effective treatment plan.
Symptom 8: Changes in skin tone or hyperpigmentation
Changes in skin tone or the appearance of dark or light patches are not always related to tanning or age-related changes. If pigmentation appears suddenly, intensifies, or is uneven, it requires evaluation by a dermatologist.
Most common causes include:
- post-inflammatory changes after acne or rashes;
- hormonal disorders, including pregnancy-related changes or endocrine imbalances;
- melasma;
- skin reactions to medications or cosmetics;
- chronic skin diseases.
Patches with blurred borders that change color or are accompanied by other symptoms—dryness, itching, or thickening of the skin—are particularly concerning. In such cases, it is important not to conceal the issue with skincare products but to determine the cause.
Symptom 9: Changes in nails and the skin around them
Nail changes are often overlooked, although they can be an early sign of dermatologic or systemic problems. Brittleness, changes in color, thickening of the nail plate, or inflammation around the nails should not be viewed as purely cosmetic.
Warning signs include:
- changes in nail color, spots, or streaks;
- thickening, crumbling, or splitting of the nail plate;
- redness, cracks, or scaling of the skin around the nails;
- pain or discomfort in the nail area;
- no improvement with cosmetic care.
These symptoms may be associated with fungal infections, eczema, psoriasis, or other skin conditions. In some cases, nail changes accompany chronic dermatologic processes and require long-term treatment.
Symptom 10: Lumps or “bumps” under the skin
Subcutaneous lumps may appear gradually and cause no discomfort for a long time. However, any lump that grows, changes shape, or becomes painful requires medical evaluation.
Signs to pay attention to include:
- a firm lump under the skin;
- gradual increase in size;
- pain, redness, or warmth of the skin over the lump;
- a change in consistency over time;
- the appearance of multiple lumps at once.
Such changes may be benign (lipomas, atheromas, cysts), but sometimes they are a manifestation of inflammation or oncologic pathology. It is not possible to determine the nature of a lump on your own, and delaying diagnosis may complicate further treatment.
Why you shouldn’t delay a visit to a dermatologist
The skin is not only a protective barrier between the body and the environment, but also a sensitive indicator of overall health. It can react to internal disturbances such as:
- hormonal imbalances;
- immune reactions;
- infectious processes;
- nutrient deficiencies;
- chronic stress.
The challenge is that different skin diseases can have very similar external manifestations. The same spot or rash may be a symptom of contact dermatitis, a fungal infection, an autoimmune process, or an allergic reaction. Without professional assessment, it is difficult to identify the true cause of changes, and incorrect treatment often leads to chronicity or complications.
Self-treatment is a separate risk. Using ointments “based on a friend’s advice” or online recommendations may temporarily reduce symptoms but not eliminate the underlying cause. In some cases, it blurs the clinical picture, making it harder for the doctor to establish an accurate diagnosis. In addition, uncontrolled use of hormonal or antibacterial agents can worsen the disease course and cause adverse effects.
It is important to remember that skin diseases are often part of a broader pathological process in the body. Timely consultation with a dermatologist helps not only address external manifestations but also identify the root cause, prevent disease progression, and choose safe and effective treatment.
Frequently Asked Questions
If a mole has changed slightly but does not hurt, is it dangerous?
Yes, pain is not a mandatory sign of dangerous changes. Alterations in shape, color, size, or borders of a mole should be a cause for concern even in the absence of pain or discomfort. Such changes may indicate a pathological process, so a dermatology consultation is needed as early as possible to rule out risks.
How can you tell that a rash is not an allergy but something more serious?
If a rash does not disappear after eliminating a possible allergen, spreads, changes its appearance, or is accompanied by itching, pain, or a general decline in well-being, it may be a non-allergic condition. In such cases, it is important not to experiment with treatment but to consult a dermatologist.
Do hormones affect skin condition?
Hormonal changes have a significant impact on skin condition. They can trigger rashes, dryness, increased oiliness, pigmentation, or exacerbation of chronic dermatoses. Such changes are often observed during pregnancy, puberty, or in endocrine disorders and require a comprehensive assessment.
What should be done if a rash appears after taking medications?
A rash after taking medications may be a manifestation of a drug reaction. It is important not to continue self-treatment and not to mask symptoms with topical products. A physician should be consulted to assess the nature of the rash, determine its association with the medication, and adjust treatment if necessary.
Can fungal infections resemble other skin diseases?
Yes, fungal infections often mimic dermatitis, psoriasis, or allergic rashes. They may be accompanied by scaling, redness, and itching. Without laboratory diagnostics, it can be difficult to differentiate them, and self-treatment may lead to a chronic course.
How often should moles be checked by a dermatologist?
In the absence of complaints, a preventive mole examination is recommended once a year. If there is a large number of pigmented lesions, a family history, or noticeable changes, examinations may be required more frequently. Regular monitoring allows potentially dangerous changes to be detected at an early stage.
Can stress cause skin problems?
Chronic or acute stress affects the immune and hormonal systems, which can provoke rashes, itching, and exacerbations of psoriasis, eczema, or acne. In such cases, treatment should be comprehensive and include not only skin care but also lifestyle modification.


















