Information in this article is provided for educational purposes only and is not a guide to self-diagnosis or treatment. If you experience any symptoms of illness, please consult a doctor.
What is thrombosis?
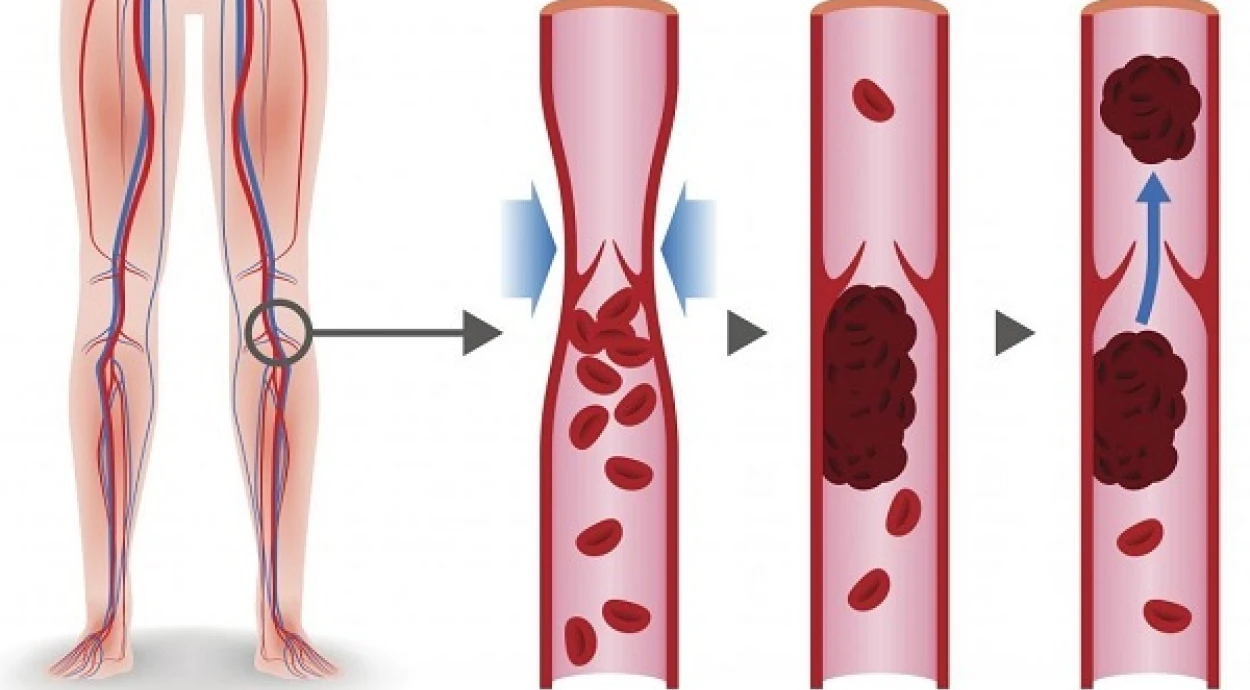
Thrombosis is the formation of blood clots (thrombi) inside blood vessels. Normally, this is a natural protective reaction of the body to vascular injury: blood coagulates near the damaged area, forming a clot that stops bleeding.
However, due to certain diseases, this mechanism may be triggered even without bleeding. In such cases, thrombi can detach and block the lumen of large vessels.
In this article, the term “thrombosis” refers to deep vein thrombosis (DVT) of the lower limbs.
Thrombosis vs. thrombophlebitis
Thrombi may form because of impaired blood clotting, damage to vessel walls, or inflammation of the venous wall. When the inflammation affects the surface veins, the condition is called thrombophlebitis. Varicose veins, which mostly involve the subcutaneous veins, cause stretching and inflammation of venous walls, creating conditions for thrombus formation.
Deep vein thrombosis is a more serious condition than thrombophlebitis. It affects veins located deeper in the tissues, most often in the calf or thigh area. Deep vein thrombosis of the legs is more dangerous because thrombi tend to be larger and can block the lumen of major arteries, including the pulmonary artery.
Causes of thrombosis
Deep vein thrombosis (DVT) may develop due to a variety of factors, including:
-
age — people over 60 are more likely to develop venous thrombosis;
-
cancer — especially malignant tumors of the intestine and pancreas;
-
smoking, including passive smoking;
-
conditions that cause increased blood clotting;
-
taking certain hormonal medications (estrogens, oral contraceptives);
-
lack of physical activity;
-
limb injuries;
-
excess body weight;
-
pregnancy and childbirth;
-
past surgical interventions.
Symptoms of deep vein thrombosis
The signs of deep vein thrombosis are nonspecific, meaning they do not always indicate a clot as the cause. Most often, patients report:
-
tenderness along the veins;
-
dull pain in the limb;
-
swelling of the entire leg — the affected leg may be 3 cm or more larger in circumference than the healthy one;
-
redness of the skin.
The intensity and frequency of these symptoms vary from person to person.
Some may also experience discomfort in the calf muscles when bending the ankle with a straightened knee. In some cases, body temperature rises to subfebrile levels (37°–37.9°C).
Possible complications
Deep vein thrombosis of the lower limbs is dangerous because thrombi can detach and travel through the bloodstream, potentially blocking a vessel. Blockage of the pulmonary artery by a thrombus is called pulmonary embolism (PE). Without adequate treatment of deep vein thrombosis, about 3 out of 100 patients die from PE.
Other serious consequences include chronic venous insufficiency, post-thrombotic syndrome, or, in rare cases, venous gangrene. Infection of the thrombus is also possible, though uncommon.
Thrombosis may also recur, especially in patients with persistent risk factors, such as cancer. For those with temporary risk factors (immobility, injury, surgery), the risk of recurrence is low.
Diagnosis of venous thrombosis
While a doctor can suspect deep vein thrombosis based on physical examination, the primary diagnostic method is venous ultrasound — Doppler or duplex scanning.
Ultrasound helps visualize the vein and assess blood flow. In common cases, such as femoral or popliteal vein thrombosis, the accuracy of ultrasound exceeds 90%. For calf or iliac vein thrombosis, it is slightly lower.
A blood test for D-dimer, a product of fibrin breakdown, is also commonly used. Its presence indicates that a thrombus recently existed in the bloodstream.
Another diagnostic option is venography, which involves injecting a contrast agent into the veins. It is typically used when ultrasound fails to locate the thrombus. However, due to its invasiveness, radiation exposure, and risk of allergic reaction, venography is performed less often. Ultrasound remains a safe and comfortable alternative.
Treatment of venous thrombosis
Drug therapy includes anticoagulants, which prevent new clots from forming, though they increase the risk of bleeding. Thrombolytic drugs, which dissolve existing clots, are also used but carry similar bleeding risks.
Treatment duration varies — from three to six months in mild cases, and lifelong in others.
A surgical option involves inserting a vena cava filter into the inferior vena cava to capture clots. The filter can be permanent or temporary and removed after several months.
In severe cases, surgical removal of the clot (thrombectomy) may be necessary.
Prevention of deep vein thrombosis
Prevention is especially important for bedridden patients recovering from major surgery or severe illness. The doctor will assess the risk of thrombosis and prescribe appropriate preventive measures.
Reducing periods of immobility is one of the main preventive steps. Anticoagulants may also be prescribed. Some patients benefit from intermittent pneumatic compression, where special sleeves rhythmically compress the legs to improve circulation.
Lifestyle changes are also recommended — increasing physical activity and reducing body weight through proper diet.
Prognosis
The prognosis is favorable if the disease is detected early and appropriate treatment is started promptly.
Frequently asked questions
Who is at risk of thrombosis?
Older adults, women after pregnancy and childbirth, oncology patients, and people with excess weight are most at risk.
Why is venous thrombosis dangerous?
Because the thrombus can detach and block vital blood vessels, which can be life-threatening.
How long does treatment last?
If the cause is temporary, therapy usually lasts up to 6 months. If the cause is permanent, treatment may be lifelong.
Which doctor treats thrombosis?
A phlebologist or vascular surgeon. In most cases, phlebologists are qualified vascular surgeons.
What test detects thrombosis?
A blood test for D-dimer is the main indicator, though nonspecific — it confirms that a thrombus recently existed but doesn’t show its location. Therefore, medical consultation and further diagnostics are required.