Treatment of endometrial hyperplasia
Endometrial Hyperplasia Treatment in Kiev
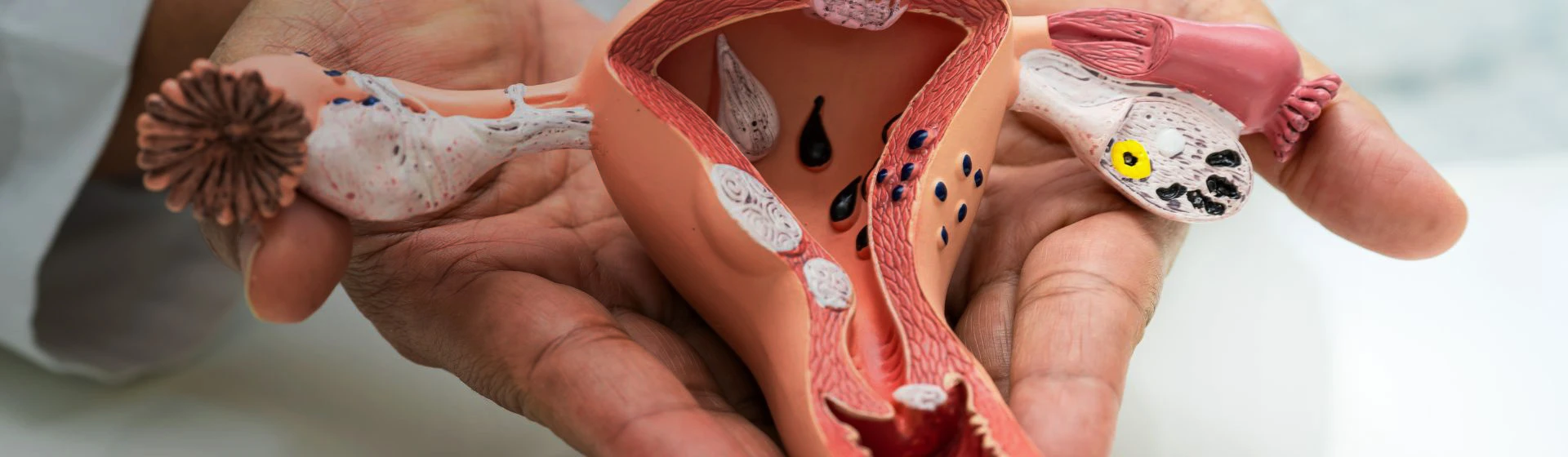
Endometrial hyperplasia is the excessive growth of the uterine lining, which is composed of endometrial cells. It most often develops due to hormonal imbalances. The condition may affect the entire endometrial surface or specific areas. Depending on the extent of hyperplasia, the presence of atypical cells, and the patient’s age, treatment can be either conservative (hormonal therapy) or surgical.
Symptoms of endometrial hyperplasia
Endometrial hyperplasia presents with distinct symptoms. However, the manifestations may vary depending on the specific characteristics of the disease.
The main symptoms include:
-
Menstrual irregularities (irregular cycles, menstruation lasting more than 5–7 days, heavy bleeding);
-
Bleeding in the middle of the menstrual cycle;
-
Bleeding during menopause and postmenopause;
-
A feeling of heaviness or dull pain in the lower abdomen;
-
Pain during and after sexual intercourse.
Significant blood loss may also lead to anemia, which causes chronic fatigue, dizziness, and pale skin.
If the condition is due to progesterone deficiency, the woman may experience general weakness, mood swings, depression, headaches, and weight gain. If estrogen levels are elevated, symptoms may include swelling, high blood pressure, increased blood clotting, mastopathy, and other disorders.
Causes of endometrial hyperplasia
Throughout the menstrual cycle, endometrial tissue undergoes phases of growth and shedding. Initially, under the influence of estrogen, it thickens to prepare for implantation of a fertilized egg and embryo development. If conception does not occur after ovulation, endometrial cells are shed, and menstruation begins.
In the second half of the cycle, estrogen production decreases while progesterone levels rise. A hormonal imbalance and, consequently, menstrual irregularities can trigger endometrial hyperplasia.
Risk factors for the condition include:
-
Hormonal imbalances;
-
Endocrine system disorders;
-
Altered function of hormone-sensitive endometrial receptors;
-
Immune system diseases;
-
Metabolic disorders;
-
Certain liver and gallbladder diseases;
-
Obesity;
-
Absence of pregnancy and childbirth;
-
Pregnancy termination;
-
Use of certain hormonal medications;
-
Smoking and alcohol consumption.
Types of endometrial hyperplasia
Endometrial hyperplasia treatment
Depending on the tissue structure and the form of growths, the following types are identified:
-
Polyps – individual overgrown endometrial areas appear in the uterine cavity;
-
Glandular hyperplasia – the layered structure of the endometrium disappears, and numerous unevenly distributed glands of various shapes appear;
-
Glandular-cystic hyperplasia – cystic formations develop;
-
Atypical hyperplasia – atypical cells appear in the endometrial tissue.
Hyperplasia is also categorized based on the extent of tissue involvement:
-
Simple – the endometrium grows evenly across the entire surface;
-
Adenomatous – uneven thickening of the hypertrophied endometrium;
-
Polypoid – spherical growths up to 1.5 cm appear on the endometrium;
-
Focal – individual pathological zones up to 6 cm in diameter develop on the endometrium.
Some experts classify adenomatous hyperplasia as atypical since it involves cells uncharacteristic of healthy endometrial tissue.
Diagnosis of endometrial hyperplasia
During the initial consultation, a gynecologist reviews the patient's complaints and performs a pelvic examination. Based on the findings, a preliminary diagnosis is made and confirmed with laboratory and instrumental tests.
The first diagnostic step for endometrial hyperplasia is transvaginal ultrasound, performed on specific days of the menstrual cycle. The doctor evaluates the structure and density of the endometrium, checking whether they correspond to the norm for that cycle day. The exam helps detect abnormalities but cannot differentiate between benign and atypical growths.
To determine the type of hyperplasia, especially the presence of atypical cells, histological analysis of a tissue sample is necessary. The simplest way to obtain this sample is via Pipelle biopsy—a minimally invasive, quick, and painless procedure. The gynecologist inserts a thin tube (up to 3 mm in diameter) into the uterine cavity and collects a small piece of endometrial tissue. The test confirms or refutes the diagnosis and detects atypical cells.
In some cases, additional diagnostics such as X-ray, CT scan of the pelvis, or hysteroscopy with targeted biopsy may be needed. Hysteroscopy is an endoscopic procedure that allows visual inspection of the uterine cavity, tissue sampling, and, if necessary, removal of polyps, altered endometrium, or other growths.
For general assessment, the doctor may also prescribe bacteriological analysis of a urogenital swab and scraping, complete blood and urine tests, and blood hormone panels.
Endometrial hyperplasia treatment at Oxford Medical
Treatment of hyperplasia is comprehensive and includes both surgical and conservative methods. The obstetrician-gynecologist develops a treatment plan based on the patient’s age, reproductive intentions, and presence of comorbidities.
In most cases, the pathological layer of endometrial tissue is first removed using hysteroscopy, where an endoscope is inserted into the uterus through the vagina. The procedure is performed under general or local anesthesia. During surgery, the doctor may perform curettage, remove growths, and collect samples for histological analysis.
In rare cases, hysterectomy (removal of the uterus) may be recommended for postmenopausal women with atypical hyperplasia and other health issues.
Hormonal therapy is usually the next step. Women of reproductive age are prescribed medications to normalize the ovarian-menstrual cycle and hormone levels, and to prevent further endometrial growth. In perimenopause, the doctor may recommend accelerating the onset of menopause with appropriate medications.
In cases of minor endometrial involvement, the gynecologist may initiate hormonal therapy without prior surgery. Surgical treatment is also rarely used for teenage girls.
Symptom management and treatment of related diseases are crucial, as hyperplasia often co-occurs with endocrine, autoimmune, and other disorders.
Hyperplasia treatment is a multistage process that must be managed by a highly qualified and experienced gynecologist. Such specialists work at Oxford Medical. The clinic is equipped with modern diagnostic and surgical equipment from Europe, allowing for precise diagnosis and gentle, minimally invasive operations.
Complications of endometrial hyperplasia
If widespread hyperplasia is not treated properly and in time, it can lead to serious consequences:
-
Uterine bleeding;
-
Anemia;
-
Menstrual cycle disturbances;
-
Infertility;
-
Malignant tumors.
According to World Health Organization statistics, 30% of patients with atypical hyperplasia and 5% without atypia develop malignancy. However, in most cases, the disease is successfully treated with surgery and hormone therapy.
Prevention of endometrial hyperplasia
The development of hyperplasia is linked to other diseases and hormonal or immune disorders. Therefore, prevention requires maintaining the health not only of the reproductive organs but of the entire body.
To reduce the risk of disease, it is recommended to:
-
Maintain hormonal balance;
-
Timely treat urogenital diseases;
-
Regularly visit a gynecologist;
-
Undergo routine check-ups.
Early diagnosis allows for easier treatment and helps prevent complications.
With timely medical attention, endometrial hyperplasia is successfully treated. Therapy helps relieve unpleasant symptoms, reduce the risk of complications, and preserve fertility.
To schedule a consultation with an obstetrician-gynecologist, call our contact center or message us in the chat.
Our doctors








Let's take care
about your health:






