Laser treatment of rectal fistula
Laser Treatment of Rectal Fistula in Kyiv
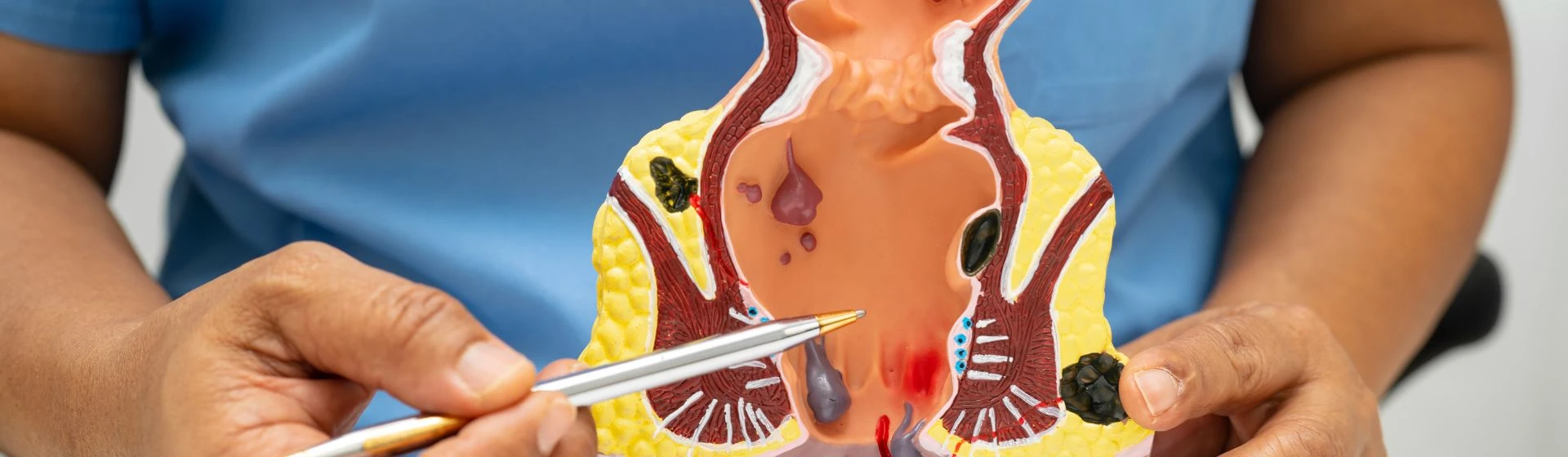
A rectal fistula is an abnormal opening that forms in the perianal area as a result of a pathological process. It begins in the rectum and may have one exit (incomplete fistula) or two (complete fistula), opening externally near the anus or internally into the lower part of the rectum (internal fistula).
How common is rectal fistula?
In European countries, rectal fistula is diagnosed in 10–25 people per 100,000 population. The disease most often affects people of working age. Among patients, men outnumber women by 2 to 3 times.
It is also worth noting that in 30–50% of cases, a fistula develops as a complication of acute paraproctitis.
Causes of rectal fistula
In most patients, the formation of a fistula is associated with an acute course of paraproctitis — an inflammatory lesion of the pararectal tissue, i.e. the tissues surrounding the rectum. It develops due to infection by E. coli, enterococcus, Staphylococcus aureus, or other bacteria.
As a result of paraproctitis, abscesses form, and parts of the mucosa, muscles, and subcutaneous tissue are affected. Scar tissue forms at the site of inflammation, creating a connective tissue capsule that confines the inflammation zone. All of this contributes to the development of a rectal fistula.
In addition to paraproctitis, risk factors for fistula formation include:
-
immune system diseases;
-
diabetes mellitus;
-
obesity;
-
perineal injuries (childbirth, etc.);
-
anal fissures and hemorrhoids;
-
constipation;
-
poor hygiene;
-
sedentary lifestyle.
Symptoms of rectal fistula
Symptoms depend on the type and location of the fistula. In the early stages, symptoms may be absent, and the patient only occasionally feels discomfort in the rectum and anus. This is also due to alternating periods of exacerbation and remission in paraproctitis.
Symptoms of rectal fistula may include:
-
formation of a fistulous opening in the perineal area;
-
discharge of pus, blood-tinged fluid, or feces from the fistula (if external) or from the rectum;
-
a foreign body sensation in the anal area (in incomplete fistula);
-
redness and inflammation of the skin around the anus;
-
pain and itching in the perineal area;
-
pain during defecation;
-
constipation;
-
impaired tone and function of the anal sphincter;
-
fever, weakness, and other general symptoms.
Types of rectal fistulas
Fistulas are classified according to several criteria.
Depending on the presence and location of the second opening, fistulas are divided into:
-
incomplete — one internal opening in the rectum;
-
complete — two openings: one in the rectum and one externally near the sphincter;
-
internal — both openings are within the rectum.
Complete fistulas are also divided into anterior, posterior, and lateral based on their relation to the sphincter.
Depending on the location relative to the external sphincter:
-
intersphincteric — located beneath the sphincter;
-
transsphincteric — involves the sphincter and surrounding tissue;
-
extrasphincteric — located in the pelvic space, exits externally in the perineal area.
There are 4 stages of extrasphincteric fistulas, depending on the presence of scar tissue, inflammation in the tissue, and the presence of purulent foci.
If not treated in time, a fistula can lead to abscess formation, sepsis, rectal scarring, and weakening of the perineal and anal muscles, which in turn may cause fecal incontinence.
Diagnosis of rectal fistula
A proctologist can diagnose a rectal fistula during a visual and digital rectal examination. To clarify the size, location, and any associated proctological conditions, instrumental diagnostics are used.
Diagnostic methods include:
-
external visual examination;
-
digital rectal examination;
-
anoscopy, rectoscopy, and/or colonoscopy — endoscopic examinations of the rectum;
-
ultrasound diagnostics;
-
fistulography — X-ray with contrast (used for extrasphincteric fistulas).
Non-surgical treatment of rectal fistula
Previously, rectal fistulas were treated exclusively with surgery. About 10 years ago, a new method emerged that allows achieving the same results without surgery — laser thermoclosure of the fistulous tract. It is widely used in Western countries, and in Ukraine, this equipment is available in only a few clinics, including Oxford Medical.
Laser treatment using the FiLaC method (Fistula-tract Laser Closure) is effective for all types of fistulas. The procedure is performed under local anesthesia. First, the proctologist cleans the fistulous tract, then applies laser energy to its walls. As a result, the tract seals shut, and over time, connective tissue and an elastic scar form in its place.
FiLaC enables fistula removal without surgical incisions or trauma to surrounding tissues. The procedure is virtually painless and has a short recovery period. It is usually performed on an outpatient basis, though hospitalization for 1–2 days may be required in some cases. Patients can return to normal life within 2–8 days.
Compared to classical surgery, FiLaC has significantly fewer contraindications and complications due to the absence of incisions, blood loss, and the destruction of all pathogenic bacteria by the laser.
At Oxford Medical, laser treatment of rectal fistulas is performed using a new German Biolitec system. It allows effective laser procedures even in complex cases.
Our doctors






Let's take care
about your health:






