skin flaking of varying intensity;
Lesions with significant thickening of the stratum corneum. The surface is rough, with pronounced keratinisation. May be accompanied by flaking or cracks.
Actinic keratosis is a skin lesion that develops under the influence of ultraviolet radiation. It manifests as skin roughness and flaking on exposed areas of the body. At first glance, the changes may seem minor; however, you should not neglect a visit to the doctor, since there is a risk of complications.
At the «Oxford Medical» clinic, patients can undergo accurate diagnostics and treatment of actinic keratosis in line with modern protocols. Our doctors analyse not only the nature of the lesion, but also the factors that contributed to its appearance, which makes it possible to choose the optimal therapeutic approach and prevent further progression of the disease.
If you have noticed symptoms of keratosis, contact the specialists of «Oxford Medical» – we will provide high-quality diagnostics and effective treatment in comfortable conditions.
You can make an appointment by phone or via the online booking form.
The main mechanism of solar keratosis development is chronic ultraviolet damage to cells, which leads to their atypical behaviour and disruption of the normal keratinisation process.
The key contributing factors include:
Taking these factors into account helps assess the risk of developing and recurring solar keratoma and to build an effective prevention strategy.
Solar keratosis may present differently depending on the duration of the lesion and individual skin characteristics. Symptoms develop gradually, so the first signs often go unnoticed.
If the following symptoms appear, it is recommended to see a doctor:
skin flaking of varying intensity;
dryness and roughness of the skin on certain areas;
appearance of cracks on affected zones;
a feeling of discomfort, irritation or mild burning.
Actinic keratosis of the skin most often forms on areas that have been exposed to sunlight for a long period of time.
The most common localisations of actinic keratosis are:
Lesions usually occur on exposed areas that have been subjected to prolonged sun exposure. Keratomas on the face are common; they form in zones with the highest insolation and may have a different appearance depending on the degree of keratinisation. Keratosis on the hands is no less frequent, as the skin of the forearms and the backs of the hands remains open and is more vulnerable to ultraviolet radiation.
In dermatology, actinic keratosis is classified according to clinical manifestations, that is, by how the lesion looks on the skin, how pronounced the keratinisation is, and so on. This classification helps assess the activity of the process and determine the optimal treatment method.
The main clinical types of actinic keratosis include:
Lesions with significant thickening of the stratum corneum. The surface is rough, with pronounced keratinisation. May be accompanied by flaking or cracks.
Flat, barely noticeable foci with reduced epidermal thickness. Flaking is mild or absent. Often has a light shade and can easily go unnoticed at early stages.
Foci with darker colouring – from light to dark brown. May resemble other pigmented lesions, therefore requires differential diagnosis.
Dense lesions with a matte surface and fine, plate-like flaking. They have well-defined borders and an uneven texture.
Lesions elevated above the skin surface with a papillomatous, granular or warty surface. They often occur in cases of pronounced photodamage.
Foci with marked thickening and dense structure, sometimes with deep keratinisation. They may crack and cause discomfort.
Actinic keratosis is a precancerous condition that develops as a result of cumulative ultraviolet damage to skin cells. Gradual structural changes in the epidermis may lead to disruption of the normal keratinisation process, which over time increases the risk of malignant neoplasms. Special attention is paid to lesions on the lips, where actinic cheilitis may develop – a condition with an increased risk of malignancy and a more aggressive course.
In addition to the risk of malignancy, actinic keratosis may have other consequences. Over time, lesions can enlarge, spread to new areas and evolve into thicker and more persistent forms of keratinisation, which complicates further treatment. Patients may develop chronic cracks and superficial skin defects, which increase the risk of secondary infection.
Such complications indicate progression of photodamage and require timely evaluation by a dermatologist. Early detection of actinic keratosis significantly reduces the risk of malignant transformation and allows the use of gentle and effective treatment methods.
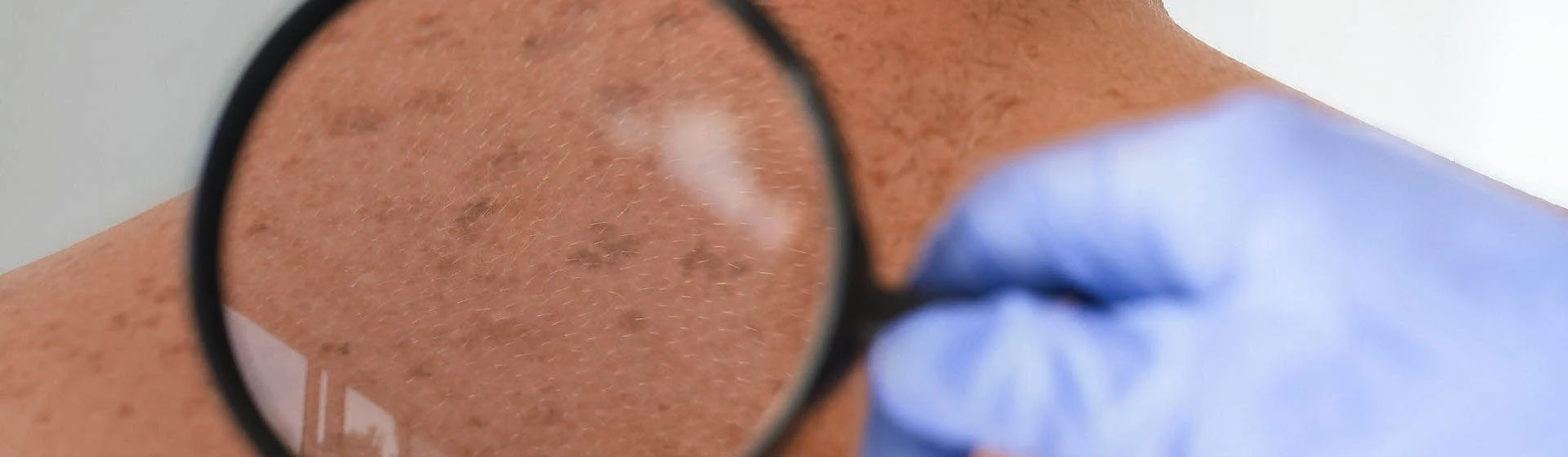
Diagnostics of actinic keratosis is based on a combination of clinical examination and instrumental methods that allow a detailed assessment of the lesion structure and differentiation from other conditions with similar features. During the examination, the doctor performs differential diagnosis with other conditions that may have a similar appearance, for example with manifestations such as keratoderma on the hands, which require a completely different therapeutic approach.
An important method for detecting actinic keratosis is dermatoscopy, which makes it possible to examine the skin under magnification and identify characteristic signs: uneven keratinisation, pigmentation changes, specific vascular patterns and microstructure of the epidermis. Dermatoscopic criteria help accurately determine the type of keratosis and assess its potential activity.
In situations when clinical and dermatoscopic data are insufficient or there is a suspicion of malignant transformation, histological examination may be recommended. Biopsy makes it possible to confirm or exclude dysplastic changes and determine the extent of tissue involvement.
Accurate diagnostics is a key step in choosing the treatment strategy, since different forms of actinic keratosis require an individual approach and careful follow-up.
Treatment of actinic keratosis is selected individually, taking into account the number of lesions, the degree of keratinisation and the general condition of the skin. In modern dermatology, a comprehensive approach is used, which may combine topical therapy, device-based methods and dermatological procedures aimed at removing pathologically altered cells.
It can be used as a standalone method or as part of a combination regimen. Most commonly, the following are prescribed:
The type, regimen and intensity of treatment are determined exclusively by a dermatologist.
The patient may be prescribed:
The following may also be recommended in keratosis:
In many cases, the highest effectiveness is achieved by combining several methods: for example, cryotherapy + topical therapy or laser + agents that normalise keratinisation. This approach makes it possible to take account of skin characteristics, minimise the risk of recurrence and ensure a more predictable outcome.
Proper skin care is an important component of the comprehensive approach to treating actinic keratosis. It helps reduce irritation, support the skin barrier, enhance treatment effects and prevent new lesions. Recommendations are selected individually; however, there are general principles that all patients are advised to follow.
Key care rules:
Sun protection is a key element of care. Daily use of high-SPF products is recommended, even on cloudy days. This helps reduce the risk of new lesions and slow the progression of existing ones.
Moisturising and emollient products help relieve dryness, reduce flaking and support normal cell renewal. Products are selected by a dermatologist according to the skin condition and its sensitivity.
In some cases, products that promote gentle removal of excessive horny layer may be recommended. This helps reduce the thickness of keratinisation and increase the effectiveness of primary treatment.
Mechanical rubbing, the use of harsh scrubs, aggressive cleansers or home peels is not recommended. Such actions may provoke irritation and worsen the condition of the affected area.
The total cost of treating actinic keratosis depends on the complexity of the disease and the chosen type of therapy. After conducting a comprehensive diagnosis, a dermatologist draws up an individual treatment program. In some cases, a dermatologist consultation is required. Make an appointment with a doctor now. You can find out the prices for services here. At Oxford Medical you will receive high-quality medical services in Kyiv and Irpen.
Keratosis is a group of conditions in which the keratinisation process of skin cells is impaired. They may present as indurations, flaking or changes in texture. Some forms develop due to ultraviolet exposure, others are associated with age, genetic factors or chronic irritation. A dermatologist’s examination is needed to determine the type of keratosis.
The treatment strategy depends on the type of keratosis and the condition of the skin. The doctor may prescribe topical agents, procedures to reduce keratinisation or methods for removing affected areas. In some cases, combination regimens are used.
Treatment may include cryotherapy, laser removal, chemical peels, curettage or the use of topical agents. The method is chosen depending on the type of lesions, their number and the sensitivity of the skin. In the case of multiple elements, the doctor may suggest a combination approach to reduce the risk of progression and recurrence.
It is not recommended to traumatise the affected areas, pick off scales, or use aggressive scrubs or peels. Sun exposure should be avoided and solarium use discontinued. Self-treatment is also dangerous, as it may mask lesions or promote progression. Treatment must be prescribed by a dermatologist.
Actinic or solar keratosis is treated by a dermatologist. The doctor performs an examination and dermatoscopy, determines the type of lesion and suggests the optimal treatment method.
The main factor is prolonged ultraviolet exposure. Spread of lesions may also be promoted by frequent sunburns, fair skin phototype, age, weakened immunity and outdoor work. Without proper sun protection, the process may progress, and lesions may enlarge or appear on new areas of the skin.
In most cases, actinic keratosis responds well to treatment. Modern methods make it possible to remove affected areas and normalise the condition of the skin. However, control of ultraviolet exposure is essential, as new elements may appear over time. Regular check-ups and prevention help maintain stable results.
Keratosis develops due to disruption of the keratinisation process in skin cells. Causes may include ultraviolet damage, age-related changes, genetic predisposition, chronic friction or exposure to chemical irritants. Some forms of keratosis are associated with specific skin or immune system characteristics. The exact type is determined during a dermatologist’s examination.







