the appearance of pink-red areas with well-defined borders on the skin;
The most common form, in which clearly defined inflammatory plaques covered with dry silvery scales form on the scalp. The lesions may extend beyond the hairline.
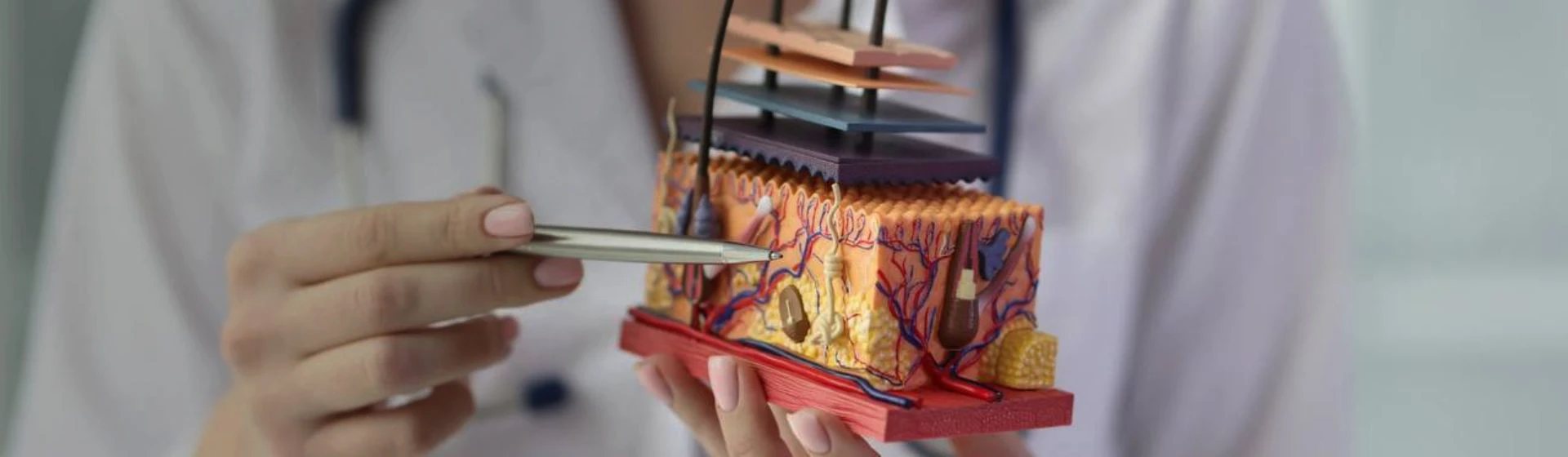
Scalp psoriasis is a chronic immune-mediated inflammatory skin disease in which areas of redness and scaling appear. Because the lesions are often “hidden” in the hair, people may mistake the early symptoms of scalp psoriasis for dandruff or irritation after hair coloring for a long time. Patients usually seek medical help only when itching and discomfort become pronounced and begin to interfere with everyday life.
If you are concerned about changes in the scalp or if symptoms recur regularly, it is advisable to schedule a consultation with a dermatologist to establish an accurate diagnosis and select an appropriate treatment regimen.
Scalp psoriasis belongs to chronic immune-mediated inflammatory diseases, the mechanisms of which are associated with dysregulation of the immune response and accelerated renewal of skin cells.
The causes of scalp psoriasis cannot be reduced to a single factor; most often, a combination of genetic predisposition and the influence of external and internal triggers is identified.
Genetic predisposition plays an important role: if close relatives have psoriasis or other autoimmune diseases, the risk of developing the condition increases. At the same time, heredity alone does not mean that symptoms will inevitably occur — additional triggering mechanisms are usually required to initiate the process.
The main risk factors include:
It is important to understand that psoriasis is not an infectious disease and is not transmitted through contact.
The manifestations of the disease may vary — from mild scaling to pronounced
inflammation with persistent itching. Symptoms often appear gradually, so at the early stages they can easily be confused with other dermatological conditions.
The most common manifestations of scalp psoriasis include:
the appearance of pink-red areas with well-defined borders on the skin;
a feeling of tightness, skin irritation, scaling;
itching, which may intensify after washing the hair or during periods of stress;
the formation of dense plaques that may extend beyond the hairline.
Psoriasis can affect different areas of the scalp, and the localization of lesions is not the same in all patients. In some cases, psoriasis develops within the hair, making skin changes visually unnoticeable. In other patients, lesions are concentrated in specific zones: psoriasis on the occipital area is quite common, where the skin is subject to additional friction, as well as psoriasis on the temples, which may spread beyond the hairline and be particularly noticeable.
It is important to understand that the intensity of symptoms does not always correspond to the size of the affected area. Even small lesions can significantly affect well-being and quality of life; therefore, the appearance of any persistent scalp changes is a reason to consult a dermatologist.
Depending on the clinical manifestations, several main forms of scalp psoriasis are distinguished, which differ in the nature of the lesions and the course of the disease.
The most common form, in which clearly defined inflammatory plaques covered with dry silvery scales form on the scalp. The lesions may extend beyond the hairline.
This form is characterized by less pronounced redness but intense scaling, which is why it often resembles seborrheic dermatitis and requires careful differential diagnosis.
By the extent of involvement, any of these forms may be limited or widespread.
Psoriasis has a chronic, relapsing course and goes through several successive stages regardless of the clinical form of the disease. Understanding the stage of the process makes it possible to assess inflammatory activity and plan scalp psoriasis treatment more effectively.
The following stages are distinguished:
Psoriasis is a chronic disease with a recurrent course. The stages of the disease may repeat throughout life, alternating with each other and forming periods of exacerbation and remission. Even after symptoms decrease, the disease may become active again under the influence of provoking factors; therefore, regular follow-up with a dermatologist and maintenance therapy play an important role in controlling the course of the disease.
During the consultation, the physician performs an examination and evaluates the nature of the lesions, their localization, borders, the presence of scaling, redness, and itching, and also clarifies how long the symptoms have been present and whether similar manifestations have occurred before.
In most cases, the diagnosis is made clinically, that is, based on external signs and medical history.
If necessary, differential diagnosis is carried out with other scalp conditions that may have similar manifestations, including seborrheic dermatitis, fungal infections, or contact dermatitis. In complex or atypical cases, the physician may recommend additional examinations, including a skin biopsy, but this method is used infrequently.
The treatment strategy for scalp psoriasis depends on the stage of the disease, the severity of the inflammatory process, and the extent of involvement.
In the progressive stage of scalp psoriasis, treatment includes the use of:
In the stationary stage, when new lesions do not appear, as well as during the regressive period, when inflammation gradually decreases and scaling becomes less pronounced, treatment is aimed at stabilizing the skin condition. During this period, the following may be used:
In scalp psoriasis, treatment may be supplemented with systemic therapy in cases of widespread involvement, frequent exacerbations, or insufficient effectiveness of topical agents. Drug treatment for scalp psoriasis is prescribed individually and may include medications that affect immune-inflammatory processes and metabolic mechanisms in the body.
A separate place in the comprehensive treatment of the scalp is occupied by non-pharmacological methods, in particular phototherapy. Dermatology at Oxford Medical is equipped with high-quality phototherapy equipment, so you can undergo the procedure in our clinic.
Treatment of a chronic condition such as scalp psoriasis requires an individualized approach and the selection of an optimal therapeutic strategy. The cost of scalp psoriasis treatment depends on the stage of the disease, the severity of symptoms, and, accordingly, the selected treatment methods. More detailed information on these issues can be provided by the physician during the appointment.
You can review the price of a dermatologist consultation in advance here. Schedule an appointment at a time convenient for you. In our clinics, you can receive high-quality medical services in Kyiv and Irpin.
Scalp psoriasis is a chronic immune-mediated inflammatory disease. It manifests as redness, scaling, plaque formation, and itching. The disease has a relapsing course with periods of exacerbation and remission and requires systematic treatment.
Psoriasis treatment is selected individually depending on the stage and severity of symptoms. In scalp psoriasis, treatment usually includes the use of topical anti-inflammatory agents and medicated shampoos. In more severe cases, phototherapy or systemic medications may be used under medical supervision.
Scalp psoriasis appears as areas of redness with well-defined borders covered with dry scales. In the early stage of psoriasis, symptoms may be minimal and resemble dandruff, but over time pronounced scaling, itching, and plaque formation along the hairline develop.
When scalp psoriasis develops, possible causes include genetic predisposition, impaired immune regulation, the effects of stress, hormonal changes, and other provoking factors. It should be noted that the disease is not associated with infection and does not occur due to poor hygiene.
No, psoriasis is not a contagious disease and is not transmitted through contact. It is impossible to contract it through touch or by sharing towels or combs. The disease is associated with internal immune mechanisms and hereditary predisposition, not with viruses or bacteria.
Seborrheic dermatitis usually presents with greasy scaling without clear borders and responds quickly to antifungal shampoos. Psoriasis is characterized by dense plaques, dry scales, and a persistent course. An accurate distinction can only be made by a dermatologist during an examination.







